On May 25, the U.S. Attorney’s Office in the Eastern District of Pennsylvania announced that Complete Physician Services, Kenneth Wiseman, DO, and Steven Schmidt, DO (collectively, “CPS”), have agreed to pay $1.5 million plus interest to resolve False Claims Act (FCA) allegations that they misrepresented the severity of illness and services rendered to increase reimbursement from multiple Medicare programs.
According to the government’s allegations, CPS submitted unsupported diagnoses to Medicare which enabled them to receive inflated reimbursements. In particular, CPS submitted claims to Medicare for patients with morbid obesity and chronic obstructive pulmonary disease (“COPD”) in cases where the government alleges that the diagnoses were not medically supported or supported by appropriate medical documentation. The government’s allegations against CPS also included “inappropriate” billings to physicians where in at least one case the physician in question was out of the country.
United States Attorney Jacqueline C. Romero said that “Almost half of Medicare beneficiaries are now enrolled in Medicare Advantage plans. Investigation of credible allegations of fraud impacting it is more important than ever.” Maureen R. Dixon, Special Agent in Charge for the U.S. Department of Health and Human Services, Office of the Inspector General added that “Today’s settlement shows our attention to and commitment in investigating all potential allegations of fraud against the Medicare Part C Programs, no matter the size of the physician practice, or the complexity of the scheme.”
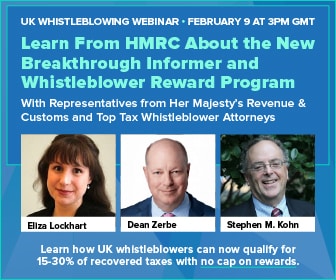
The alleged violations came to the government’s attention through a former CPS employee who blew the whistle and filed a civil suit under the qui tam provision of the FCA. Qui tam claims enable private citizens to file lawsuits on behalf of the government if they know of an individual or company defrauding the government. Qui tam whistleblowers are eligible to receive between 15 and 30% of the government’s recovery. The whistleblower’s share in this case has not been made public at this time.
U.S. Attorney Romero emphasized the role that whistleblowers play in catching and deterring potential healthcare fraud: “Detecting fraud is much easier when we have the cooperation of whistleblowers like the ones in this case.”