Generic pharmaceutical manufacturers, Taro Pharmaceuticals USA, Inc., Sandoz Inc. and Apotex Corporation, will pay $447.2 million to settle allegations that they conspired to artificially inflate the price of multiple generic drugs. According to a U.S. Department of Justice (DOJ) press release, this conspiracy allegedly resulted in higher than normal drug prices for federal medical programs and their beneficiaries.
The government alleged that by communicating with each other and agreeing on generic drug prices, these three companies both paid and received illicit compensation through cooperation. Under the Anti-Kickback Statute of the False Claims Act, this kind of cooperation can be considered a kickback. According to the press release, this kickback scheme allegedly took place between 2013 and 2015.
The agreed upon settlements for this case demonstrate the seriousness of the alleged False Claims Act violations, with Taro Pharmaceuticals agreeing to pay $213.2 million, Sandoz paying $185 million, and Apotex on the line for $49 million. The drugs implicated in the alleged kickback scheme range from hypertension and cholesterol treatment drugs to arthritis treatment medications, and even include antifungal and skin treatment creams.
Artificially inflating the prices of generic drugs through conspiracy jeopardizes the ability of individuals to continue to use medication that makes their lives safer and more comfortable. Raising drug prices to artificially high levels also erodes trust in the pharmaceutical and greater American medical system, damaging reputations and relationships between the public and medical professionals. Inflating prices through collusion damages Medicare and other federal medical programs by tricking the government into paying more for necessary medical services and wasting taxpayer dollars.
“Conspiring to raise prices on generic medications is illegal and could prevent patients from being able to afford their needed prescription drugs. Americans have the right to purchase generic drugs set by fair and open competition, not collusion,” said Special Agent in Charge Maureen R. Dixon of the Philadelphia Regional Office of the Inspector General, Department of Health and Human Services (HHS-OIG). “HHS-OIG along with our law enforcement partners will continue to investigate allegations of companies engaging in actions that put the public and the Medicare program at risk.”
Another aspect of the settlement requires all three companies to enter five-year Corporate Integrity Agreements (CIAs). These agreements are designed to increase oversight over future high level corporate decisions and develop systems for increased transparency within each organization. All three companies will also have to implement “compliance measures including risk assessment programs, executive recoupment provisions and compliance-related certifications from company executives and board members.”
While a whistleblower was not mentioned in the settlement, this action shows the strength and relevancy of the False Claims Act, even when a whistleblower is not involved. The False Claims Act and it’s essential medical elements like the Stark Act and Anti-Kickback provisions are the backbone of the U.S.’s defense against medical fraud.
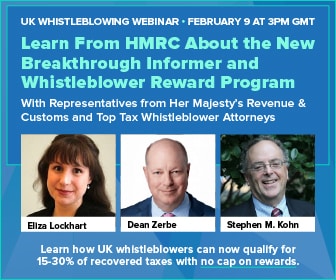
Whistleblowers often make large disclosures in cases like this one, and reap large percentages of the settlements as a reward for doing so. In a qui tam action against a company violating the False Claims Act and defrauding the government, whistleblowers are entitled to 15 to 30% of the total recovered amount.