On December 19, the Department of Justice announced that Community Health Network, an Indiana non-profit health network, agreed to pay the United States $345 million to resolve allegations that it violated the False Claims Act.
The government alleges that Community Health Network knowingly submitted claims to Medicare for services that were referred in violation of the Stark Law, which prohibits hospitals from billing certain services referred by physicians with whom the hospital has financial relationships unless the relationship meets one of the law’s statutory or regulatory exceptions.
According to the United States’ complaint, Community Health Network began an illegal scheme in 2008 and 2009 to recruit physicians for employment to take their “downstream referrals.” The network allegedly successfully recruited hundreds of local physicians, including cardiovascular specialists, neurosurgeons, and breast surgeons, by paying them salaries that were much higher than what they were receiving in their private practices.
The complaint further alleged that Community knew the compensation figures it provided to the valuation firm it hired to analyze the compensation it proposed paying to its recruited specialists were false. The network allegedly ignored repeated warnings from the valuation firm regarding the legal perils of overcompensating its physicians.
This case stemmed from a qui tam whistleblower lawsuit filed by Community Health Network’s former Chief Financial and Chief Operating Officer, Thomas Fischer. Qui Tam enables private citizens to file lawsuits on behalf of the government if they know of an individual or company defrauding the government. When qui tam suits result in successful action against a fraudulent company or individual, qui tam whistleblowers are eligible to receive between 15 and 30% of the government’s recovery.
In this case, the qui tam whistleblower share has not been determined yet.
According to Principal Deputy Assistant Attorney General Brian Boynton, “Today’s historic recovery follows several years of litigation. It demonstrates the Justice Department’s continued commitment to combatting healthcare fraud. We are focused on ensuring that physicians provide objective medical advice to their patients – advice that is not tainted by improper financial relationships. More generally, we will continue to use the False Claims Act to protect the integrity of federal healthcare programs and to prevent the waste and abuse of taxpayer funds.”
On July 25, a bipartisan group of senators introduced the False Claims Amendments Act of 2023, which address a few technical loopholes undermining the success of the FCA. The bill is widely supported by whistleblower advocates.
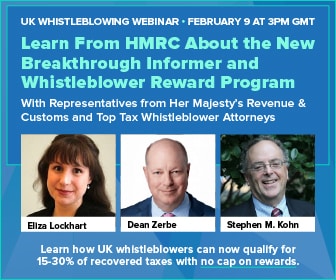
“The False Claims Act is America’s number one fraud-fighting law,” said whistleblower attorney Stephen M. Kohn. “These amendments are urgently needed to ensure that whistleblowers can continue to play their key role in protecting taxpayers from corporate criminals.”
Further Reading:
Indiana Health Network Agrees to Pay $345 Million to Settle Alleged False Claims Act Violations
Bipartisan Legislation Unveiled to Strengthen False Claims Act