American Senior Communities, L.L.C., or ASC, will pay $5,591,044.66 to settle allegations that it submitted false claims to Medicare and thus violated the False Claims Act. The case stemmed from a 2017 whistleblower complaint, which alleged that “ASC had engaged in conduct to defraud the Medicare program,” the U.S. Department of Justice (DOJ) press release states.
ASC provides “skilled nursing and long-term care services throughout Indiana.” The whistleblower, who was “a former employee of a hospice services company doing business with ASC,” filed their complaint “under the False Claims Act in the United States District Court for the Southern District of Indiana.” The whistleblower also alleged “that ASC was charging Medicare directly for various therapy services provided to beneficiaries who had been placed on hospice, when those services should have already been covered by the beneficiaries’ Medicare hospice coverage.”
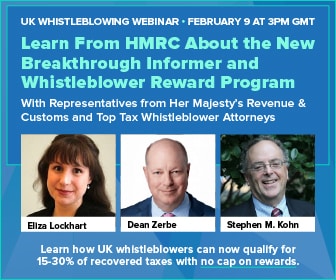
The qui tam provisions of the False Claims Act enable private citizens to file lawsuits on behalf of the government if they know of an individual or company defrauding the government. Qui tam whistleblowers are eligible to receive between 15 and 30% of the government’s recovery, if one occurs.
According to the press release, “the estimated loss to the Medicare program was $2,795,522.33.”
“Whistleblowers are critical to protecting public funds from fraud, waste, and abuse,” said U.S. Attorney Zachary A. Myers. “Health care providers who submit false claims or otherwise violate state and federal regulations when billing the United States Government will face consequences.
Whistleblowers are key to uncovering corruption and misconduct in the healthcare industry: fraudulent schemes can be particularly harmful to patients and erode trust in the medical system. In Fiscal Year 2021, qui tam whistleblowers helped the DOJ recover $1.6 billion in settlements. The DOJ highlighted health care fraud as “the leading source of the department’s False Claims Act settlements and judgments.”