An Oklahoma City specialty hospital, its management group, a physician’s group, and two physicians will pay over $72.3 million to settle allegations of improper payments to physicians under the False Claims Act. The allegations center around a scheme to give kickbacks from the Oklahoma Center for Orthopedic and Multi-Specialty Surgery (OCOM) and the Oklahoma City branches of management company United Surgical Partners (USP) to physician’s group Southwest Orthopedics Specialist (SOS) in return for patient referrals to OCOM. These kickbacks increased referrals to OCOM and resulted in false claims to Medicare, Medicaid, and TRICARE.
Between 2006 and 2018, OCOM and USP allegedly provided incentives to SOS to increase patient referrals to OCOM. Some of these incentives took the form of excessive compensation for services or under market-value office space. Other incentives included selling equity to doctors and guaranteeing buyback of those stocks. OCOM and USP also allegedly gave preferential investment opportunities to some doctors in exchange for referrals. All of these actions constitute kickbacks under the Anti-Kickback Statute. By providing these kickbacks to SOS, USP allegedly compromised physicians’ ability to make decisions solely based on their patients’ best medical interests. Kickback schemes like this one can be extremely damaging to the quality of care in our medical system: they influence doctors to provide treatment based on incentives instead of the best medical practice. These schemes hurt the most vulnerable, such as veterans and those who receive Medicare and Medicaid.
USP agreed to pay $60.86 million to the United States, $5 million to the State of Oklahoma, and $206,000 to the State of Texas, resolving alleged offering of investment opportunities to physicians in Texas. SOS and two of its physicians, Anthony L. Cruse, D.O. and R.J. Langerman, Jr., D.O., will also pay $5.7 million to the U.S. and $495,619 to the State of Oklahoma.
Both OCOM and SOS also agreed to enter five-year Corporate Integrity Agreements (CIAs) to ensure their good behavior. These CIAs require that OCOM and SOS hire an Independent Review Organization to watch over the relationships of both companies’ executives. The agreements will help prevent improper payments and relationships. The CIAs also require key executives of OCOM and SOS to earn compliance-related certifications to increase accountability.
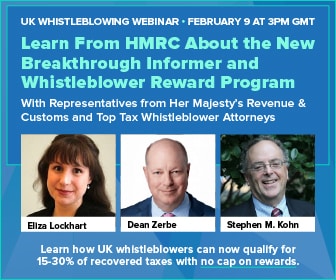
A whistleblower initially filed a complaint under the qui tam, or whistleblower provisions, of the False Claims Act and the government intervened in the case. The False Claims Act allows whistleblowers, or relators, to sue on behalf of the federal or state government. Relators can be eligible for monetary rewards for providing the government with solid evidence of fraud. In this case, the unnamed whistleblower will receive 15 to 30% of the total funds recovered. This settlement serves as another example of the False Claims Act working as intended and rooting out corruption from the inside.
Read the DOJ press release: Oklahoma City Hospital, Management Company, And Physician Group To Pay $72.3 Million To Settle Federal And State False Claims Act Allegations Arising From Improper Payments To Referring Physicians