On August 18, the U.S. Department of Justice (DOJ) announced four settlements involving healthcare providers and organizations in California. Four entities will pay $70.7 million to settle allegations “that they violated the federal False Claims Act and the California False Claims Act by submitting or causing the submission of false claims to Medi-Cal related to Medicaid Adult Expansion under the Patient Protection and Affordable Care Act (ACA).
According to the press release, “[t]he civil settlements include the resolution of claims” brought by qui tam whistleblowers. The whistleblowers are Atul Maithel and Andre Galvan, both of whom formerly worked for one of the entities that is engaging in a settlement.
The qui tam provisions of the False Claims Act enable private citizens to file lawsuits on behalf of the government if they know of an individual or company defrauding the government. Qui tam whistleblowers are eligible to receive between 15 and 30% of the government’s recovery, if one occurs.
The press release explains that as part of the ACA, Medi-Cal, which is California’s Medicaid program, was expanded in January 2014 “to cover the previously uninsured ‘Adult Expansion’ population.” This includes “adults between the ages of 19 and 64 without dependent children with annual incomes up to 133% of the federal poverty level.” For the first three years of the program, the “federal government fully funded the expansion coverage.” In order to comply with California’s Department of Health Care Services (DHCS), California county organized health systems (COHS) had to pay the state a certain amount of money if it “did not spend at least 85% of the funds it received for the Adult Expansion population on ‘allowed medical expenses.’” The state of California would then have to pay back the money from a COHS to the federal government.
The settlements, then, resolve allegations that four healthcare providers and organizations “knowingly submitted or caused the submission of false claims to Medi-Cal for ‘Additional Services’ provided to Adult Expansion Medi-Cal members between Jan. 1, 2014, and May 31, 2015.”
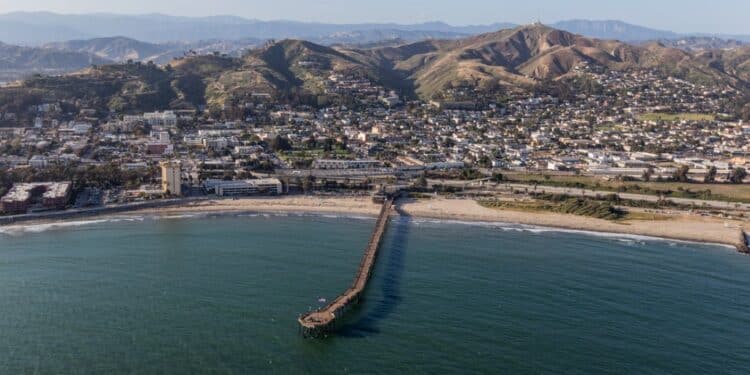
The four entities involved in the $70.7 million settlement are “Ventura County Medi-Cal Managed Care Commission doing business as Gold Coast Health Plan (Gold Coast), a county organized health system (COHS) that contracts to arrange for the provision of health care services under California’s Medicaid program (Medi-Cal) in Ventura County, California; Ventura County, which owns and operates Ventura County Medical Center, an integrated health care system that provides hospital, clinic, and specialty services; Dignity Health (Dignity), a not-for-profit hospital system that operates two acute care hospitals in Ventura County; and Clinicas del Camino Real Inc. (Clinicas), a non-profit health care organization located in Ventura County.”
As part of the settlements, “Gold Coast will pay $17.2 million to the United States; Ventura County will pay $29 million to the United States; Dignity will pay $10.8 million to the United States and $1.2 million to the State of California; and Clinicas will pay $11.25 million to the United States and $1.25 million to the State of California.”
The settlement agreements involving Clinicas and Dignity both state: “Conditioned upon receiving the Settlement Amount payments the United States shall pay to Relators by electronic funds transfer 18.5 percent and California shall pay to Relators by electronic funds transfer 24 percent of each such payment received under the Settlement Agreement as soon as feasible after receipt of each such payment.” The settlement agreement with Ventura County omits the second part of the above statement and only includes information about the U.S. paying the whistleblowers “18.5% of each such payment received under the Settlement Agreement.”
According to the press release, Maithel, one of the whistleblowers, was “Gold Coast’s former controller,” while the other whistleblower Galvan was “Gold Coast’s former director of member services.”